Data Shows Childhood Vaccination Rates Backsliding in the U.S.

The U.S. is witnessing a concerning trend in public health: childhood vaccination rates are declining. This backsliding has significant implications for the health and wellbeing of children across the country.
Recent data investigation reveals that this trend is not only a minor fluctuation but a notable shift in a public health trend that had previously shown steady progress.
Key Takeaways
- Vaccination rates among children in the U.S. are decreasing.
- This decline poses serious risks to public health.
- The trend indicates a need for renewed focus on vaccination programs.
- Understanding the causes of this backsliding is crucial.
- Addressing the issue will require a multifaceted approach.
The Alarming Trend in U.S. Childhood Immunization
Childhood vaccination data analysis shows an alarming trend in the U.S. Recent immunization statistics indicate a decline in vaccination rates among children, raising concerns among healthcare professionals and public health officials.
Recent Statistical Evidence
According to the latest healthcare analytics, there has been a noticeable drop in the vaccination coverage for various childhood vaccines. This trend is evident across different datasets and regions, suggesting a widespread issue.
Key statistics include:
- A decline in MMR vaccination rates
- Reduced coverage for DTaP vaccines
- Other critical vaccines showing similar trends
Comparison to Historical Vaccination Coverage
Historical data shows that U.S. childhood vaccination rates had been steadily improving over the past few decades. However, recent immunization statistics reveal a reversal of this trend, with vaccination rates now declining.
Initial Public Health Responses
In response to these alarming trends, public health officials have begun to implement measures to address the decline. These include enhanced public awareness campaigns, improved access to vaccination services, and community outreach programs.
By understanding the current state of childhood immunization and comparing it to historical data, we can better appreciate the need for immediate action to reverse this trend and protect public health.
Data Investigation: Childhood Vaccination Rates are Backsliding Across the U.S.
New evidence suggests that vaccination coverage among children in the United States is backsliding. A comprehensive analysis of national datasets has uncovered a concerning trend in declining childhood vaccination rates across various regions.
Methodology of the Investigation
The investigation into childhood vaccination rates employed a multi-faceted approach to data collection and analysis. Reliable data sources were utilized to ensure the accuracy and relevance of the findings.
Data Sources and Collection Methods
Data for this investigation was sourced from national immunization surveys and healthcare provider records. These sources provided a comprehensive overview of vaccination trends across different demographics and geographic locations.
Statistical Analysis Techniques
Advanced statistical analysis techniques were applied to identify trends and patterns in the vaccination data. Regression analysis and time-series analysis helped in understanding the dynamics of vaccination coverage over time.
Key Findings from National Datasets
The analysis revealed significant declines in vaccination rates for several key vaccines. According to the data, there has been a notable decrease in the coverage of MMR (Measles, Mumps, Rubella) and DTaP (Diphtheria, Tetanus, Pertussis) vaccines among children aged 2-5 years.
“The decline in vaccination rates is a public health concern that requires immediate attention. As healthcare providers, it’s crucial we address the root causes of this trend.”
Verification and Validation Processes
To ensure the accuracy of the findings, the data underwent rigorous verification and validation processes. Cross-validation techniques were used to check the consistency of the data across different sources.
The investigation’s results underscore the need for targeted interventions to restore vaccination coverage to pre-pandemic levels. By understanding the factors contributing to the decline, public health officials can develop more effective strategies to improve childhood vaccination rates.
Historical Context of U.S. Vaccination Programs
The history of vaccination programs in the U.S. is a complex narrative of medical advancements and public health challenges. Over the years, the standards for childhood immunization have evolved significantly, shaped by scientific breakthroughs, public health policies, and societal attitudes.
Evolution of Childhood Immunization Standards
The development of vaccines against major childhood diseases has been a cornerstone of public health in the U.S. The introduction of vaccines for diseases such as measles, mumps, and rubella (MMR) and diphtheria, tetanus, and pertussis (DTaP) has dramatically reduced the incidence of these conditions.
Previous Periods of Vaccination Hesitancy
Despite the successes, there have been periods of vaccination hesitancy. For instance, concerns over vaccine safety in the late 1990s and early 2000s led to a decline in vaccination rates in some communities. Understanding these historical trends is crucial for addressing current challenges.
Successful Public Health Campaigns of the Past
Public health campaigns have played a vital role in promoting vaccination. Notable examples include nationwide initiatives to vaccinate against polio and measles. These campaigns not only increased vaccination coverage but also helped to educate the public about the importance of immunization.
Geographic Disparities in Vaccination Coverage
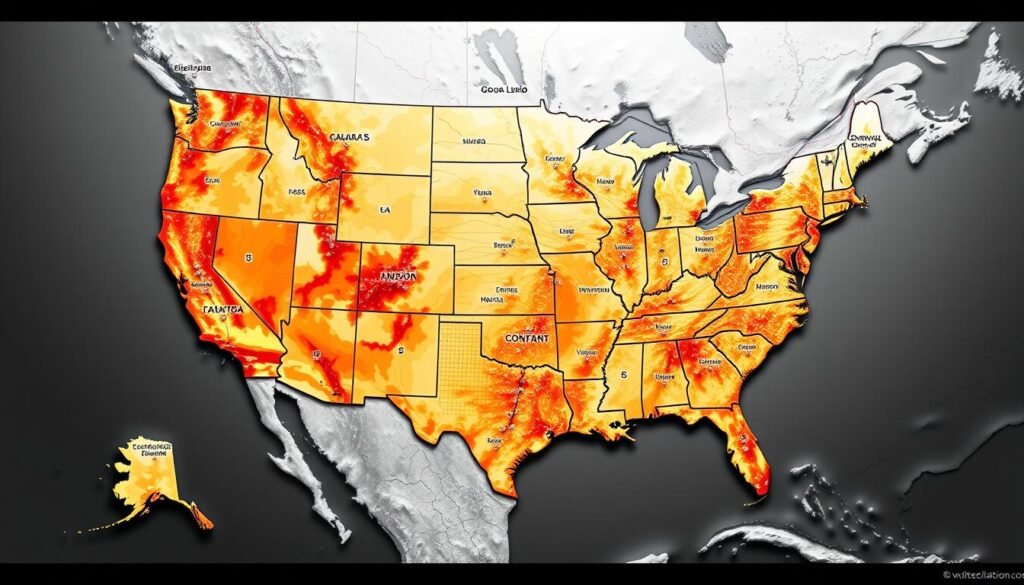
Geographic differences in vaccination rates have become a pressing concern, as data reveals uneven coverage across the country. The decline in childhood vaccination rates is a complex issue, influenced by a variety of regional factors.
States with the Steepest Declines
Some states have experienced more significant drops in vaccination rates than others. For instance, certain southern and western states have seen declines in vaccination coverage that are more pronounced compared to the national average. Data analysis is crucial in identifying these trends and understanding their causes.
Urban vs. Rural Vaccination Patterns
The distinction between urban and rural vaccination patterns is another critical aspect. Generally, rural areas tend to have lower vaccination rates compared to urban centers, largely due to differences in healthcare access and socioeconomic factors.
Socioeconomic Factors Influencing Regional Variations
Socioeconomic factors play a significant role in vaccination coverage. Income and education levels are closely correlated with vaccination rates, as higher income and education often result in better health outcomes.
Income and Education Correlations
Research has shown that areas with higher average incomes and education levels tend to have higher vaccination rates. This correlation underscores the importance of addressing socioeconomic disparities to improve public health.
Healthcare Access Disparities
Access to healthcare is another critical factor influencing vaccination rates. Regions with limited healthcare infrastructure or services often struggle to maintain adequate vaccination coverage, highlighting the need for improved healthcare access.
Specific Vaccines Experiencing the Most Significant Drops
The decline in childhood vaccination rates in the U.S. is a pressing concern, with certain vaccines showing more significant drops than others. Recent healthcare analytics data highlight the vaccines that are most affected.
MMR (Measles, Mumps, Rubella) Vaccination Trends
The MMR vaccine has seen a notable decline in coverage. Measles, mumps, and rubella are highly contagious diseases that can lead to serious complications, making vaccination crucial.
DTaP (Diphtheria, Tetanus, Pertussis) Coverage Analysis
DTaP vaccination rates have also dropped. Pertussis, or whooping cough, is particularly dangerous for infants, and the decline in DTaP coverage raises concerns about increased vulnerability to this disease.
Other Critical Childhood Vaccines Showing Decline
Besides MMR and DTaP, other vaccines are also experiencing declines.
Polio Vaccination Rates
Polio vaccination rates have decreased, which is concerning given the historical success of polio eradication efforts in the U.S.
Hepatitis B Immunization Coverage
Hepatitis B vaccination coverage is also declining. Hepatitis B can lead to chronic liver disease, making vaccination essential.
The trends indicate a need for targeted public health interventions to address the decline in vaccination rates for these critical vaccines.
The COVID-19 Pandemic’s Impact on Routine Childhood Immunizations
As the COVID-19 pandemic spread globally, it had a profound impact on the delivery of routine childhood immunizations. The pandemic brought about unprecedented challenges, affecting healthcare systems worldwide and leading to significant disruptions in routine immunization services.
Disruptions to Healthcare Access During Lockdowns
During the lockdowns, many healthcare facilities were overwhelmed with COVID-19 cases, leading to the reallocation of resources and staff to manage the pandemic. This shift resulted in the suspension or reduction of routine immunization services. Parents and caregivers faced difficulties in accessing vaccination services due to lockdown restrictions, fear of infection, and the closure of some healthcare facilities.
Shifting Priorities in Public Health Resources
Public health resources were redirected to combat the COVID-19 pandemic, affecting the allocation of funds and personnel for routine immunization programs. This shift in priorities led to a decrease in vaccination coverage rates. The pandemic highlighted the need for flexible and resilient healthcare systems that can adapt to emergencies while maintaining essential services.
Post-Pandemic Recovery Efforts and Their Effectiveness
In the aftermath of the pandemic, recovery efforts focused on rebuilding and strengthening immunization programs. Strategies included catch-up campaigns, enhanced outreach, and the use of digital technologies to improve vaccine delivery. These efforts have shown varying degrees of success, with some regions achieving significant improvements in vaccination coverage.
Lessons Learned for Future Public Health Emergencies
The COVID-19 pandemic provided valuable lessons for maintaining routine immunizations during public health emergencies. Key takeaways include the importance of maintaining essential health services, leveraging technology for remote healthcare delivery, and ensuring community engagement. These lessons will be crucial in preparing for future health crises and mitigating their impact on routine immunization programs.
The pandemic has underscored the need for robust public health infrastructure and the importance of maintaining routine childhood immunizations, even during times of crisis. By analyzing the impact of the COVID-19 pandemic on immunization services, we can better prepare for future challenges and ensure the continued protection of public health.
The Growing Influence of Vaccine Hesitancy
As vaccination rates decline, the issue of vaccine hesitancy has come to the forefront of public health discussions. Vaccine hesitancy refers to a delay or refusal to accept vaccines despite their availability. This growing concern is multifaceted, influenced by various factors including misinformation, changing parental attitudes, and community-specific concerns.
Social Media’s Role in Spreading Misinformation
Social media platforms have become significant conduits for the dissemination of misinformation regarding vaccines. “Anti-vaccination misinformation on social media is a major public health concern”, as noted by experts. This misinformation can lead to increased skepticism and hesitancy among parents and guardians.
Changing Parental Attitudes Toward Childhood Vaccines
Parental attitudes toward vaccines are shifting, with some expressing concerns over vaccine safety and efficacy. “The fear of potential side effects and mistrust in pharmaceutical companies are driving factors”. Understanding these concerns is crucial for public health officials to develop targeted interventions.
Community-Specific Concerns and Resistance
Different communities exhibit unique concerns and levels of resistance to vaccination. Cultural, socioeconomic, and educational factors play significant roles in shaping these attitudes. For instance, some communities may have historical or cultural reasons for mistrusting government health initiatives.
Demographic Patterns in Vaccine Hesitancy
Vaccine hesitancy is not uniform across different demographics. Certain patterns emerge when examining age, generation, political ideology, and other factors.
Age and Generation Factors
Younger parents are more likely to be influenced by social media and online forums, potentially increasing their hesitancy. In contrast, older generations may rely more on traditional sources of information.
Political and Ideological Correlations
There is evidence to suggest that political ideology and affiliation can influence vaccine hesitancy.
“Political polarization is increasingly linked to vaccination attitudes, with some political groups expressing outright opposition to mandatory vaccination.”
This correlation underscores the complexity of addressing vaccine hesitancy.
Addressing vaccine hesitancy requires a nuanced understanding of these demographic patterns and the factors influencing them. By tailoring public health strategies to specific communities and demographics, it may be possible to mitigate the decline in vaccination rates.
Public Health Implications of Declining Vaccination Rates
Declining vaccination rates pose a serious threat to public health, potentially reversing years of progress in disease prevention. The consequences of this trend are multifaceted, affecting not only individual health but also the broader healthcare system and economy.
Increased Risk of Preventable Disease Outbreaks
The most immediate concern is the heightened risk of outbreaks of diseases that were previously under control. Measles, mumps, and pertussis are among the diseases that can spread rapidly in unvaccinated populations.
- Measles can lead to serious complications, including pneumonia and encephalitis.
- Mumps can cause meningitis and orchitis.
- Pertussis, or whooping cough, can be particularly dangerous for infants.
Economic Costs to Healthcare Systems
The economic burden of declining vaccination rates is substantial. Outbreaks of preventable diseases result in increased healthcare costs, lost productivity, and strain on public health resources.
“The economic impact of vaccine-preventable diseases is significant, with costs running into billions of dollars annually.”
Vulnerable Populations at Heightened Risk
Certain populations are disproportionately affected by declining vaccination rates.
Immunocompromised Children
Children with weakened immune systems are more susceptible to serious infections and may not be able to receive certain vaccines.
Infants Too Young for Vaccination
Infants who are too young to be vaccinated rely on herd immunity for protection against diseases.
Herd Immunity Thresholds and Current Coverage
Herd immunity is achieved when a sufficient percentage of a population is immunized, protecting those who are not vaccinated.
Maintaining high vaccination coverage is crucial to prevent outbreaks and protect vulnerable populations. Current trends indicate a need for improved public health strategies to address vaccine hesitancy and ensure adequate vaccine coverage.
Expert Perspectives on the Vaccination Crisis
Experts from various health organizations are sounding the alarm on the decline in childhood vaccination rates. This trend has significant implications for public health, and understanding the perspectives of experts in the field is crucial.
Insights from Pediatric Health Organizations
Pediatric health organizations have been vocal about the risks associated with declining vaccination rates. According to the American Academy of Pediatrics, the decrease in vaccination coverage poses a serious threat to the health of children nationwide.
Key concerns include the potential for outbreaks of preventable diseases and the long-term impact on children’s health.
CDC and Public Health Officials’ Statements
The Centers for Disease Control and Prevention (CDC) has issued statements highlighting the importance of maintaining high vaccination rates. Public health officials emphasize that vaccination is a critical tool in preventing the spread of infectious diseases.
- The CDC reports a decline in vaccination rates for several key vaccines, including MMR and DTaP.
- Public health officials stress the need for continued education and outreach to address vaccine hesitancy.
Academic Research on Vaccination Trends
Recent studies have investigated the factors contributing to the decline in vaccination rates. Research published in peer-reviewed journals highlights the role of misinformation and socioeconomic factors in vaccine hesitancy.
Key findings include the impact of social media on the spread of misinformation about vaccines.
International Comparisons and Global Health Perspectives
Comparing vaccination rates and policies internationally can provide valuable insights. Countries with robust vaccination programs offer lessons for addressing vaccine hesitancy and improving coverage.
The global health community is working together to address the challenges posed by declining vaccination rates. By sharing data and strategies, countries can work towards improving public health outcomes.
Conclusion: The Path Forward for U.S. Childhood Vaccination
The declining childhood vaccination rates in the U.S. pose a significant public health trend that requires immediate attention. As discussed, the backsliding immunization statistics are attributed to various factors, including the COVID-19 pandemic, vaccine hesitancy, and geographic disparities.
To reverse this trend, it’s crucial to strengthen public health infrastructure, enhance access to vaccination services, and implement targeted interventions to address vaccine hesitancy. Public health officials, healthcare providers, and communities must work together to promote the importance of childhood vaccination and provide accurate information to counter misinformation.
By understanding the complex factors influencing immunization statistics and adopting a multi-faceted approach, the U.S. can improve childhood vaccination rates, protect vulnerable populations, and maintain herd immunity thresholds. The path forward involves a concerted effort to prioritize childhood vaccination as a critical component of public health.






