Calcium Build-Up in Arteries and High Blood Pressure: Understanding the Connection
The silent progression of calcium deposits in your arteries can significantly impact your blood pressure and overall heart health. When calcium builds up in arterial walls, it restricts blood flow and forces your heart to work harder, often leading to hypertension. This dangerous combination increases your risk of heart attacks, strokes, and other serious cardiovascular events.
Fortunately, understanding the relationship between arterial calcification and high blood pressure is the first step toward taking control of your cardiovascular health. In this comprehensive guide, we’ll explore this connection and provide actionable strategies to address calcium build-up naturally.
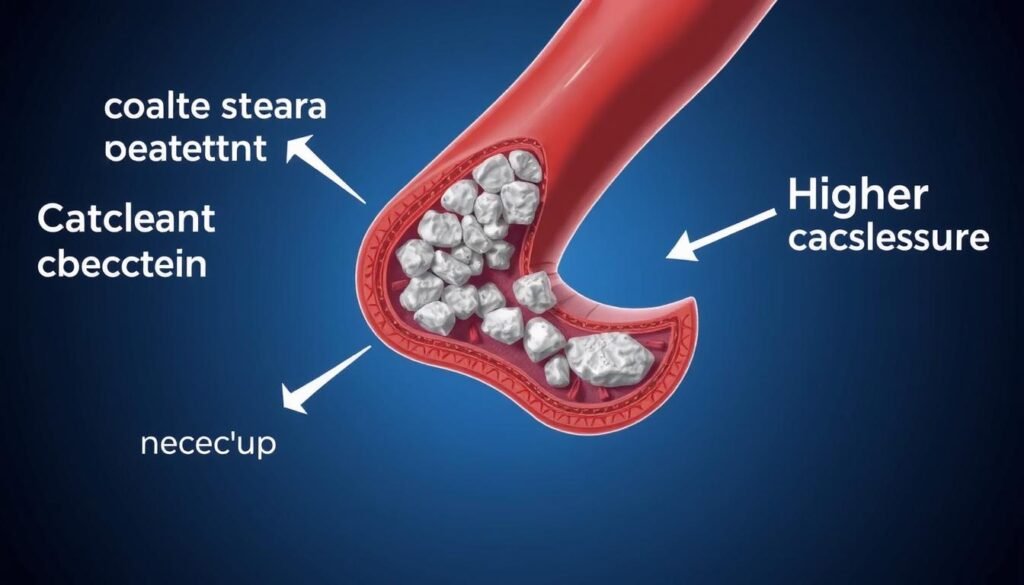
The Problem: Stiff Arteries and Hypertension
Calcium deposits narrow arterial passages, restricting blood flow and increasing pressure
What is Hypertension?
High blood pressure (hypertension) occurs when the force of blood pushing against your artery walls is consistently too high. Normal blood pressure is below 120/80 mmHg, while readings above 130/80 mmHg indicate hypertension. Left untreated, this condition damages blood vessels and vital organs.
Hypertension is often called the “silent killer” because it typically has no symptoms until significant damage has occurred. It affects nearly half of American adults and contributes to leading causes of death including heart disease and stroke.
How Healthy Arteries Function
In their optimal state, arteries are flexible tubes that expand and contract with each heartbeat. This elasticity helps maintain proper blood pressure by accommodating blood flow and reducing resistance. Healthy arterial walls have smooth inner linings that allow blood to flow freely.
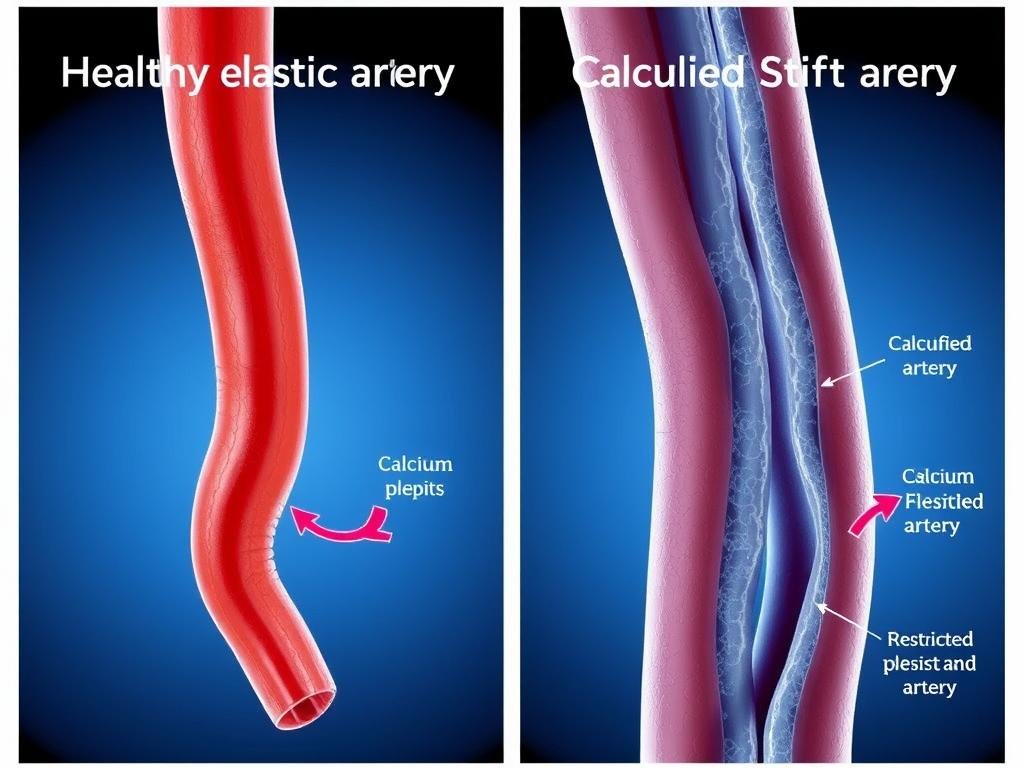
The Connection: Arterial Stiffness and Blood Pressure
When calcium accumulates in arterial walls, it creates a devastating cycle. The arteries become stiff and narrow, forcing your heart to pump harder to move blood through your body. This increased effort raises your blood pressure, which in turn causes more damage to arterial walls, leading to further calcification.
Research shows that arterial stiffness is both a cause and consequence of high blood pressure. Studies have found that people with higher coronary artery calcium scores face significantly increased risks of cardiovascular events, even when other risk factors are controlled.
The Role of Calcium in Arterial Plaque Formation
What is Arterial Plaque?
Arterial plaque is a complex substance that accumulates in artery walls. It consists of:
- Cholesterol and fatty substances
- Cellular waste products
- Fibrin (a clotting material)
- Calcium deposits
- Inflammatory cells
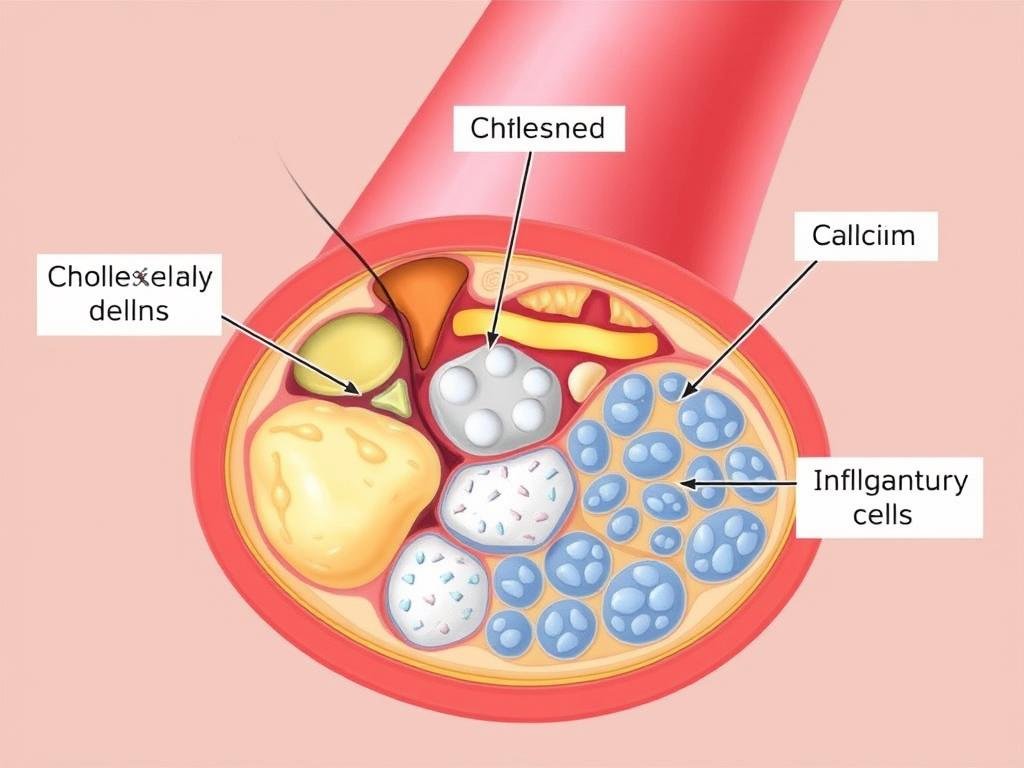
How Calcium Contributes to Arterial Hardening
Calcium plays a critical role in the progression of atherosclerosis. Initially, plaque begins as soft deposits, but over time, calcium from the bloodstream can infiltrate these areas. This process, called arterial calcification, transforms soft plaque into hard, bone-like structures that significantly reduce arterial flexibility.
The calcification process typically begins after plaque has been present for about five years. Once calcified, the plaque becomes more stable but causes the artery to lose its crucial elasticity, contributing directly to increased blood pressure.
In people older than 70, more than 90% of men and 67% of women have coronary artery calcification. This gender difference exists because estrogen helps protect women from atherosclerosis before menopause.
Dietary Calcium vs. Arterial Calcium: An Important Distinction
It’s crucial to understand that calcium in your diet is not the same as calcium deposits in your arteries. Dietary calcium from foods like dairy products is essential for bone health and normal cellular function. The calcium that builds up in arteries comes from a complex process involving inflammation, tissue damage, and disrupted calcium metabolism.
In fact, some research suggests that adequate dietary calcium with proper vitamin D and K2 intake may help prevent calcium from depositing in arteries by ensuring it goes to bones where it belongs.
Risk Factors for Arterial Calcification
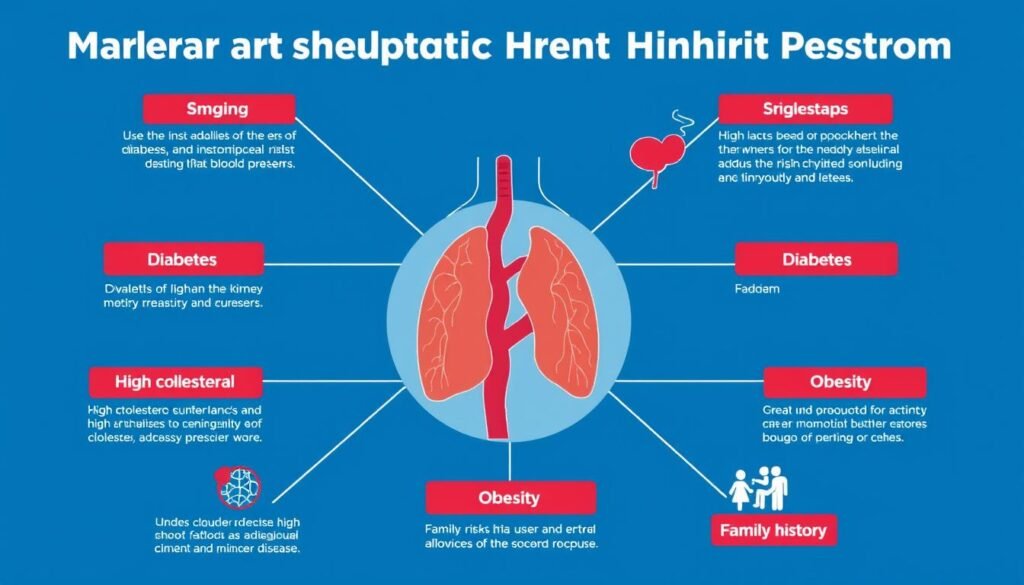
Several factors increase your risk of developing calcium deposits in your arteries:
Medical Conditions
- Diabetes mellitus – High blood glucose damages arterial walls
- Chronic kidney disease – Disrupts mineral metabolism
- High cholesterol – Especially elevated LDL and low HDL
- High blood pressure – Creates a cycle of arterial damage
Lifestyle Factors
- Smoking – Damages arterial walls and accelerates plaque formation
- Sedentary lifestyle – Reduces arterial health and elasticity
- Poor diet – High in processed foods and sodium
- Obesity – Increases inflammation and metabolic disruption
Warning Signs to Watch For
Arterial calcification often develops silently for years before symptoms appear. Potential warning signs include:
- Chest pain or pressure, especially during physical activity
- Shortness of breath with minimal exertion
- Unexplained fatigue
- Irregular heartbeat
- Numbness or weakness in extremities
If you experience these symptoms, consult a healthcare provider promptly.
Diagnosing Calcium Build-Up in Arteries
Before implementing solutions, it’s important to understand the extent of arterial calcification. Several diagnostic tests can assess calcium deposits in your arteries:
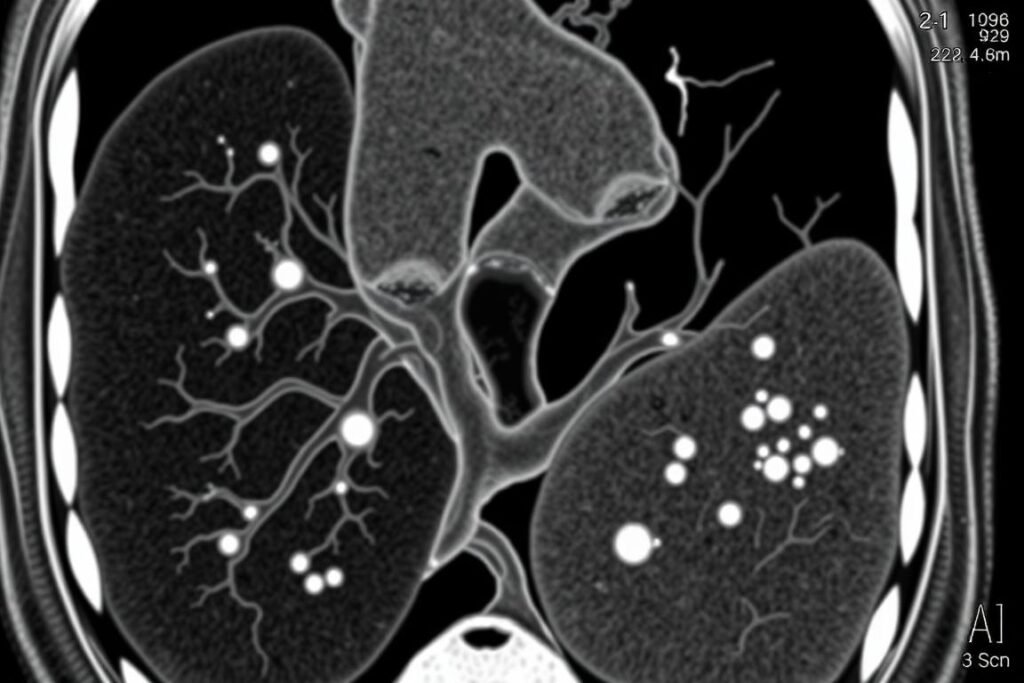
Cardiac CT scan showing calcium deposits (bright white areas) in coronary arteries
Coronary Artery Calcium (CAC) Score
This non-invasive CT scan measures the amount of calcium in your coronary arteries. Your doctor will calculate an Agatston score based on the quantity, density, and size of calcium deposits:
| CAC Score | Interpretation | Risk Level |
| 0 | No identifiable plaque | Very low risk |
| 1-99 | Mild calcification | Mild to moderate risk |
| 100-399 | Moderate calcification | Moderate to high risk |
| 400+ | Severe calcification | High risk |
When Should You Get Tested?
Consider discussing a calcium score test with your doctor if you:
- Are between 40-70 years old
- Have a family history of heart disease
- Have risk factors like high blood pressure, diabetes, or high cholesterol
- Are concerned about your cardiovascular health
Other Diagnostic Methods
For more detailed assessment, your doctor might recommend:
- Cardiac intravascular ultrasound (IVUS) – Uses sound waves to visualize inside coronary arteries
- Intravascular optical coherence tomography (IVOCT) – Uses light waves to create detailed images of arterial walls
- Angiography – Uses contrast dye and X-rays to visualize blood flow through arteries
Solutions to Manage Calcium Build-Up and High Blood Pressure

Dietary Interventions
Key Nutrients for Arterial Health
Vitamin K2
This crucial vitamin helps direct calcium to your bones where it belongs, rather than allowing it to deposit in soft tissues like arteries. Studies show K2 can reduce arterial calcification and improve elasticity.
Sources: Fermented foods like natto, certain cheeses, egg yolks, and organ meats.
Magnesium
Magnesium helps regulate calcium metabolism and relaxes blood vessels, potentially lowering blood pressure. It may help prevent calcium from depositing in soft tissues.
Sources: Dark leafy greens, nuts, seeds, whole grains, and legumes.

Beetroot for Vascular Health
Beetroot contains naturally occurring nitrates that convert to nitric oxide in the body. Nitric oxide is a powerful vasodilator that relaxes blood vessel walls, potentially lowering blood pressure and improving blood flow.
Research has shown that regular consumption of beetroot juice can reduce blood pressure by approximately 4-10 mmHg in many individuals. This effect is comparable to some blood pressure medications.
Support Your Arterial Health Naturally
Our premium beetroot supplement provides concentrated nitrates to support healthy blood pressure and improve circulation. Each capsule contains the equivalent of 6 whole beets in a convenient, easy-to-take form.
Heart-Healthy Eating Patterns
Beyond individual nutrients, your overall eating pattern significantly impacts arterial health. Consider these evidence-based approaches:

The Mediterranean diet emphasizes foods that support arterial health
DASH Diet
The Dietary Approaches to Stop Hypertension (DASH) diet was specifically designed to lower blood pressure. It emphasizes:
- Fruits and vegetables
- Whole grains
- Low-fat dairy
- Lean proteins
- Limited sodium (less than 2,300mg daily)
Mediterranean Diet
This traditional eating pattern has been linked to lower rates of heart disease and may help prevent arterial calcification:
- Abundant plant foods
- Olive oil as primary fat
- Moderate fish and seafood
- Limited red meat
- Optional moderate wine consumption
Lifestyle Modifications
Exercise for Arterial Health
Regular physical activity improves arterial function and elasticity while helping to control blood pressure. Aim for at least 150 minutes of moderate-intensity exercise weekly, including:

- Aerobic activities – Walking, swimming, cycling
- Strength training – 2-3 sessions weekly
- Flexibility exercises – Yoga, stretching
- Balance training – Especially important for older adults
Stress Management
Chronic stress contributes to inflammation and high blood pressure, potentially accelerating arterial damage. Effective stress-reduction techniques include:

- Mindfulness meditation – Even 10 minutes daily can help
- Deep breathing exercises – Practice 4-7-8 breathing (inhale for 4, hold for 7, exhale for 8)
- Regular sleep habits – Aim for 7-8 hours of quality sleep
- Time in nature – “Forest bathing” has been shown to reduce stress hormones
Important Health Considerations
While natural approaches can be effective, they should complement, not replace, medical care. Always consult your healthcare provider before:
- Starting new supplements, especially if you take medications
- Making significant dietary changes
- Beginning a new exercise program, particularly if you have existing heart disease
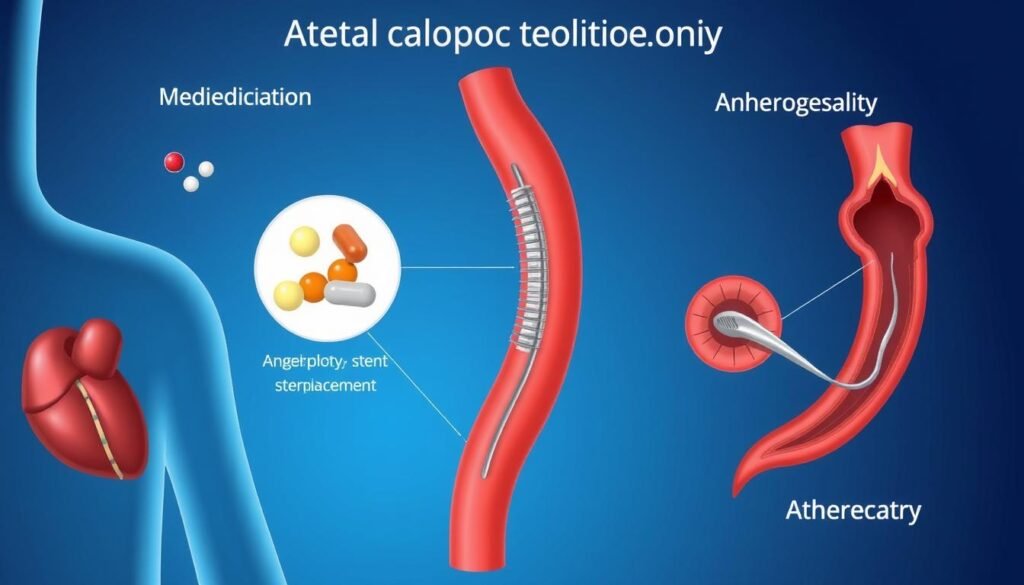
Medical Approaches to Arterial Calcification
In addition to lifestyle modifications, medical interventions may be necessary for managing calcium build-up in arteries and high blood pressure, especially in advanced cases.
Medications
Several classes of medications may help manage the conditions associated with arterial calcification:
- Statins – Help lower cholesterol and may slow progression of calcification
- Antihypertensives – Various classes of blood pressure medications
- Antiplatelet agents – Reduce risk of blood clots forming on plaques
- Calcium channel blockers – May help prevent calcium from entering cells
Interventional Procedures
For severe arterial calcification, interventional procedures may be recommended:
Intravascular Lithotripsy
This newer procedure uses pressure waves to break up calcium deposits in arteries, allowing for better stent placement. Success rates exceed 92% in appropriate candidates.
Atherectomy
Several types (rotational, orbital, laser) can physically remove plaque and calcium from arterial walls. These procedures have approximately 90% success rates.

Before and after treatment of severe arterial calcification
When to Consult a Specialist
Consider seeking specialized cardiovascular care if you:
- Have a high calcium score (100+)
- Experience symptoms like chest pain or shortness of breath
- Have multiple risk factors for heart disease
- Have difficulty controlling your blood pressure
Your Comprehensive Action Plan
Managing calcium build-up in arteries and high blood pressure requires a multi-faceted approach. Here’s a practical action plan to improve your arterial health:

Step 1: Assess Your Current Status
- Schedule a check-up to measure blood pressure and assess risk factors
- Discuss calcium scoring or other appropriate tests with your doctor
- Review your current medications and supplements
- Evaluate your diet and exercise habits honestly
Step 2: Implement Dietary Changes
- Adopt a Mediterranean or DASH eating pattern
- Increase intake of vitamin K2 and magnesium-rich foods
- Consider beetroot supplementation for nitric oxide support
- Reduce sodium to less than 2,300mg daily (ideally 1,500mg)
- Limit processed foods and added sugars
Step 3: Optimize Your Lifestyle
- Begin with 10-minute daily walks, gradually increasing duration and intensity
- Practice stress reduction techniques for at least 10 minutes daily
- Ensure 7-8 hours of quality sleep each night
- Quit smoking and limit alcohol consumption
- Maintain a healthy weight or work toward gradual weight loss if needed
Step 4: Monitor Your Progress
- Track your blood pressure regularly at home
- Keep a journal of dietary changes and how you feel
- Follow up with your healthcare provider as recommended
- Reassess calcium scores as advised by your doctor
Take Action Today for Healthier Arteries
Support your cardiovascular health with our premium beetroot supplement. Clinically studied to promote healthy nitric oxide levels, support normal blood pressure, and improve circulation.
A Note on Arterial Health and Blood Pressure
The relationship between calcium build-up in arteries and high blood pressure creates a challenging cycle that affects millions of people worldwide. By understanding this connection and taking proactive steps, you can significantly improve your cardiovascular health and reduce your risk of serious complications.
Remember that arterial calcification develops over many years, and similarly, improvements take time. Be patient with yourself as you implement changes, and celebrate small victories along the way. With consistent effort and the right approach, you can support your arterial health and work toward healthier blood pressure levels.
Always partner with healthcare professionals for personalized guidance, especially if you have existing cardiovascular conditions or take medications. The strategies outlined in this guide work best as part of a comprehensive approach that includes appropriate medical care.






