Blood Sugar Spikes: Symptoms and How to Prevent Them
Blood Sugar Spikes: Symptoms and How to Prevent Them
Stable Blood Sugar: Understanding Spikes, Identifying Symptoms, and Effective Prevention Strategies
Every day, our bodies perform an incredible dance of balance, maintaining crucial physiological parameters within narrow ranges to ensure optimal health. One such critical balance involves blood sugar, or glucose, the primary fuel source for our cells. When this balance is disrupted by frequent or severe blood sugar spikes, it can lead to a cascade of unwelcome symptoms and, over time, significant health concerns. Understanding what triggers these fluctuations, recognizing their signs, and implementing proactive strategies are vital steps toward safeguarding your well-being.
Understanding Blood Sugar and Its Crucial Role
Blood sugar, or glucose, is a simple sugar derived from the foods we eat, particularly carbohydrates. It’s the essential energy currency that powers our cells, from the brain to muscles. After we consume food, carbohydrates are broken down into glucose, which then enters the bloodstream. In response, the pancreas releases insulin, a hormone that acts like a key, allowing glucose to enter cells for energy or storage.
Maintaining stable blood sugar levels is paramount for overall health. When glucose levels are consistently too high or too low, our body’s systems struggle. Stable levels ensure a steady energy supply, support proper organ function, and contribute to metabolic harmony. This delicate balance, often unnoticed when working correctly, becomes profoundly evident when it falters.
What Exactly Are Blood Sugar Spikes?
A “blood sugar spike,” scientifically known as postprandial hyperglycemia, refers to a rapid and often significant increase in blood glucose levels shortly after eating. While it’s normal for blood sugar to rise slightly after a meal as glucose enters the bloodstream, a “spike” implies an unusually high or rapid surge that can overwhelm the body’s insulin response.
These spikes commonly occur when we consume meals rich in easily digestible carbohydrates, especially refined sugars and starches. Such foods are quickly broken down into glucose, flooding the bloodstream faster than the body can effectively manage. The pancreas works overtime to produce insulin, but if the surge is too great, or if the body’s cells are less responsive to insulin (a condition known as insulin resistance), glucose levels can climb excessively.
The immediate impact of a blood sugar spike can range from noticeable discomfort to subtle shifts in energy and mood. Over time, repeated spikes can contribute to more serious health issues, including increased risk of developing prediabetes and type 2 diabetes, cardiovascular complications, and nerve damage. Understanding the mechanisms behind these spikes is the first step toward mitigating their effects and fostering healthier glucose control.
Early Signs and Symptoms
Recognizing the early signs and symptoms of blood sugar spikes is crucial for timely intervention and long-term health. While some symptoms are quite noticeable, others can be subtle and easily dismissed, making awareness key. These symptoms can vary in intensity depending on the magnitude and duration of the glucose surge, and individual responses may differ.
#### Common Acute Symptoms
When blood sugar levels rise rapidly and significantly, the body sends clear signals. These acute symptoms often appear within an hour or two after a meal and can disrupt daily activities.
- Fatigue and Energy Crashes: One of the most frequently reported symptoms is a sudden onset of tiredness or a profound energy crash, often an hour or two after eating a high-carbohydrate meal. This isn’t just typical post-meal drowsiness; it’s a feeling of being completely drained, sometimes accompanied by a strong urge to nap. This occurs because the rapid influx of glucose triggers a strong insulin response, which then clears the glucose from the blood quickly, leading to a subsequent drop that can feel like a crash. The body struggles to maintain a steady energy supply when riding this rollercoaster of highs and lows.
- Increased Thirst and Frequent Urination: Elevated blood sugar levels mean there’s excess glucose in the bloodstream. The kidneys, in an effort to remove this excess sugar, work harder and produce more urine. This increased urination (polyuria) can lead to significant fluid loss, triggering intense thirst (polydipsia) as the body attempts to rehydrate. This cycle can be particularly pronounced during a spike.
- Blurred Vision: Temporary changes in vision, such as a slight blurring or difficulty focusing, can occur during a blood sugar spike. High glucose levels cause fluid to shift in and out of the lenses of the eyes, temporarily altering their shape and affecting their ability to focus. While usually transient, persistent or frequent blurring can be a warning sign of underlying issues.
- Headaches and Dizziness: Headaches, often described as a dull ache or throbbing sensation, can be a symptom of elevated blood glucose. This is thought to be related to changes in blood vessel dilation or hydration levels. Dizziness can also manifest as the body adjusts to rapid shifts in sugar levels and fluid balance.
- Irritability and Mood Swings: The brain is highly sensitive to fluctuations in glucose supply. When blood sugar levels spike and then drop, it can lead to mood instability, making individuals feel more irritable, anxious, or agitated than usual. The brain’s energy regulation being thrown off balance can significantly impact emotional well-being.
- Difficulty Concentrating / Brain Fog: A clear mind relies on a steady supply of glucose. During a spike, and especially during the subsequent crash, individuals may experience “brain fog,” characterized by difficulty focusing, forgetfulness, or a general haziness in thinking. Cognitive function can be temporarily impaired as the brain struggles with the abrupt energy changes.
- Increased Hunger Despite Eating: Paradoxically, despite having consumed a meal, a blood sugar spike can sometimes lead to increased hunger. This happens because insulin rapidly shuttles glucose into cells, or the cells become resistant to insulin, leaving the bloodstream cleared of sugar, yet the cells haven’t effectively utilized it for energy. The brain then signals that more fuel is needed, triggering hunger pangs even after a recent meal.
- Skin Issues: High blood sugar levels can affect skin health in various ways. One notable sign is acanthosis nigricans, a darkening and thickening of the skin, particularly in the folds of the neck, armpits, and groin. This condition is strongly associated with insulin resistance. Additionally, elevated glucose can impair the body’s healing process, leading to slow-healing cuts, scrapes, or sores, as well as an increased susceptibility to skin infections.
- Tingling or Numbness: While typically associated with long-term nerve damage (neuropathy) from chronic high blood sugar, even frequent, unmanaged spikes can, over time, contribute to subtle nerve irritation. Some individuals might experience transient tingling, numbness, or a “pins and needles” sensation in their hands or feet, which could be an early warning sign of nerve stress.
- Recurring Infections: High blood sugar creates an environment where certain pathogens, especially yeast and bacteria, can thrive. Individuals experiencing frequent urinary tract infections (UTIs), yeast infections (candidiasis), or skin infections might be unknowingly experiencing regular blood sugar spikes that compromise their immune system’s effectiveness and create hospitable conditions for microbial overgrowth.
- Weight Fluctuations: Unexplained weight gain, particularly around the abdomen, or persistent difficulty losing weight despite efforts, can be linked to insulin resistance and frequent blood sugar spikes. When insulin levels are consistently high due to spikes, the body is signaled to store more fat. Conversely, rapid blood sugar drops can trigger cravings for quick energy sources, leading to further overeating and weight management challenges.
- Digestive Upset: While not always immediately linked, chronic blood sugar imbalances can sometimes contribute to digestive issues. Gastroparesis, a condition where the stomach empties too slowly, is associated with diabetes, but even less severe digestive discomforts like bloating, gas, or inconsistent bowel movements might be influenced by how the body processes sugars and fats, or by an imbalanced gut microbiome that high sugar intake can foster.
- Refined Carbohydrates and Sugars: This is perhaps the most significant dietary culprit. Foods like white bread, pastries, sugary cereals, candy, sodas, fruit juices (without fiber), and many processed snacks contain carbohydrates that are quickly broken down into glucose. Lacking fiber, these foods are rapidly absorbed, leading to a swift and steep rise in blood sugar. For example, a can of soda can deliver over 30 grams of pure sugar, causing an immediate glucose surge.
- Lack of Fiber: Fiber, particularly soluble fiber, plays a critical role in slowing down the digestion and absorption of carbohydrates. When meals lack sufficient fiber, glucose enters the bloodstream more rapidly, increasing the likelihood of a spike. Many modern diets are deficient in fiber-rich whole foods.
- Portion Sizes: Even healthy carbohydrates, when consumed in very large portions, can lead to blood sugar spikes simply because of the sheer volume of glucose entering the system at once. A single meal with excessive amounts of pasta, rice, or potatoes, even if whole grain, can overwhelm the body’s insulin response.
- Timing of Meals: Skipping meals, especially breakfast, can lead to increased hunger later in the day, often resulting in overeating or making less healthy food choices. This “catch-up” eating can then lead to larger blood sugar spikes. Similarly, eating large, carbohydrate-heavy meals late at night, especially close to bedtime, can also contribute to elevated morning blood sugar readings as the body’s metabolism slows during sleep.
- Hidden Sugars: Many processed foods, even those not traditionally thought of as “sweet,” contain significant amounts of added sugars. Sauces, dressings, yogurts, canned soups, and even savory snacks can be laden with high-fructose corn syrup, sucrose, or other forms of sugar that contribute to unexpected glucose surges. Reading nutrition labels carefully is crucial.
- Lack of Physical Activity: Regular physical activity helps cells become more sensitive to insulin, meaning they can more efficiently absorb glucose from the bloodstream. A sedentary lifestyle reduces insulin sensitivity, making it harder for the body to manage glucose after meals, thus increasing the likelihood of spikes. Muscle contractions during exercise can also directly take up glucose from the blood without the need for insulin.
- Stress: Chronic stress is a powerful trigger for blood sugar spikes. When we’re stressed, the body releases hormones like cortisol and adrenaline. These hormones prepare the body for a “fight or flight” response by signaling the liver to release stored glucose into the bloodstream, providing quick energy. If this stress response is prolonged or frequent, it can lead to persistently elevated blood sugar levels, even without eating.
- Poor Sleep Quality: Insufficient or poor-quality sleep disrupts hormonal balance, affecting glucose metabolism. Sleep deprivation can decrease insulin sensitivity and increase levels of cortisol, both of which contribute to higher blood sugar levels. Studies show that even a few nights of inadequate sleep can impair glucose tolerance.
- Dehydration: Water plays a vital role in transporting glucose and nutrients. When the body is dehydrated, glucose in the bloodstream becomes more concentrated. Furthermore, dehydration can prompt the body to release hormones that raise blood sugar. Staying adequately hydrated supports kidney function in clearing excess glucose and helps maintain overall metabolic health.
- Certain Medications: Some medications can inadvertently elevate blood sugar levels. For example, corticosteroids (used for inflammation), certain diuretics, beta-blockers, and some psychiatric medications can interfere with glucose metabolism or reduce insulin sensitivity. It’s important to discuss potential side effects with a healthcare provider.
- Skipping Meals: While counterintuitive, skipping meals can sometimes lead to blood sugar spikes. When you go for long periods without eating, your body may compensate by releasing stored glucose from the liver to prevent hypoglycemia. However, this can set the stage for a rebound spike when you eventually eat, especially if you then overcompensate with a large, carbohydrate-rich meal. The body prefers a steady, rather than erratic, fuel supply.
- Prioritize Whole Foods: Build your diet around unprocessed or minimally processed foods. This means opting for fresh fruits, a wide variety of vegetables, lean proteins (chicken, fish, legumes, tofu), whole grains (quinoa, oats, brown rice), and healthy fats. Whole foods retain their natural fiber, vitamins, and minerals, which are crucial for healthy glucose metabolism.
- Embrace Fiber: Make dietary fiber your ally. Soluble fiber, found in oats, beans, lentils, apples, and citrus fruits, forms a gel-like substance in the digestive tract, slowing down glucose absorption. Insoluble fiber, found in whole grains, vegetables, and fruit skins, adds bulk and aids digestion. Aim for at least 25-30 grams of fiber per day from various sources. Consider starting meals with a salad or a serving of non-starchy vegetables.
- Balanced Meals: Structure your meals to include a healthy balance of protein, healthy fats, and fiber-rich carbohydrates. Protein and fat help slow down stomach emptying and glucose absorption, leading to a more gradual rise in blood sugar. For instance, instead of just a piece of fruit, pair it with a handful of nuts or a spoonful of almond butter. When having a carbohydrate-heavy meal, ensure it’s balanced with a good source of lean protein and plenty of vegetables.
- Mindful Carbohydrate Intake: While not all carbohydrates are bad, it’s essential to be mindful of their type and quantity. Focus on complex carbohydrates with a lower glycemic index (GI), such as whole grains, legumes, and non-starchy vegetables. These are digested more slowly, leading to a gentler rise in blood sugar. Be aware of portion sizes, even for healthy carbohydrates, as excessive amounts can still lead to spikes.
- Healthy Fats: Incorporate monounsaturated and polyunsaturated fats into your diet, found in avocados, olive oil, nuts, seeds, and fatty fish. These fats not only contribute to satiety but also help slow down the absorption of glucose and can improve insulin sensitivity over time.
- Meal Timing and Frequency: Instead of two or three large meals, consider eating smaller, more frequent meals throughout the day. This can help prevent extreme hunger and large blood sugar swings. Spreading your carbohydrate intake across several smaller meals can make it easier for your body to manage glucose. Try to eat meals at consistent times to establish a rhythm for your metabolism.
- Hydration: Make water your primary beverage. Staying well-hydrated helps the kidneys flush out excess sugar and keeps blood volume stable. Avoid sugary drinks, fruit juices (even “100% juice” can be high in concentrated sugars without the fiber), and sweetened teas, which can contribute significantly to blood sugar spikes.
- Vinegar Before Meals: Emerging research suggests that consuming a small amount of apple cider vinegar (e.g., 1-2 tablespoons diluted in water) before a meal, especially one rich in carbohydrates, may help to blunt the post-meal blood sugar spike. The acetic acid in vinegar is thought to slow down carbohydrate digestion and improve insulin sensitivity.
- Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, combined with two or more days of strength training. Exercise enhances insulin sensitivity, meaning your cells can take up glucose more efficiently. Even short walks after meals can be incredibly effective in lowering post-meal blood sugar levels by prompting muscles to use glucose for energy. Incorporate activities you enjoy to make it sustainable, whether it’s brisk walking, cycling, swimming, dancing, or gardening.
- Stress Management Techniques: Chronic stress elevates cortisol, a hormone that raises blood sugar. Incorporate stress-reducing practices into your daily life. This could include mindfulness meditation, deep breathing exercises, yoga, spending time in nature, listening to calming music, or engaging in hobbies. Even 10-15 minutes of dedicated relaxation can make a difference.
- Adequate Sleep: Prioritize 7-9 hours of quality sleep each night. Sleep deprivation impairs insulin sensitivity and can increase appetite-regulating hormones, leading to cravings for unhealthy foods. Establish a consistent sleep schedule, create a relaxing bedtime routine, and optimize your sleep environment to promote restful slumber.
- Weight Management: If you are overweight or obese, even a modest weight loss (5-10% of body weight) can significantly improve insulin sensitivity and help stabilize blood sugar levels. Focus on sustainable changes in diet and activity rather than restrictive crash diets.
- Limiting Alcohol Intake: Alcohol, especially sugary cocktails or beer, can contribute to blood sugar spikes. It can also interfere with the liver’s ability to produce glucose, potentially leading to low blood sugar (hypoglycemia) later, particularly if consumed on an empty stomach or in large quantities. If you drink, do so in moderation and be mindful of your choices.
- Fasting Plasma Glucose (FPG) Test: Measures blood sugar after an overnight fast. This helps identify high baseline levels.
- Oral Glucose Tolerance Test (OGTT): Involves drinking a sugary solution after a fast, followed by blood sugar measurements at specific intervals. This assesses how well your body processes glucose.
- HbA1c Test (Glycated Hemoglobin): Provides an average of your blood sugar levels over the past 2-3 months. This is a critical indicator of long-term glucose control.
- Registered Dietitians (RDs) or Certified Diabetes Educators (CDEs): These experts specialize in nutrition and diabetes management. They can help you create a personalized meal plan, teach you about carbohydrate counting, explain the glycemic index, and offer practical strategies for balanced eating to prevent spikes. They can also address specific dietary needs or concerns.
- Endocrinologists: These specialists focus on hormone-related conditions, including diabetes. If your blood sugar issues are complex, difficult to manage, or if you have other endocrine disorders, an endocrinologist can provide advanced care and specialized treatment.
- Exercise Physiologists: Can help design a safe and effective exercise program tailored to your fitness level and health goals, optimizing physical activity for glucose control.
- Experience Persistent Symptoms: If you regularly notice symptoms such as excessive thirst, frequent urination, unexplained fatigue, blurred vision, or recurring infections, even after making some initial lifestyle adjustments, it’s crucial to get these checked. These could be indicators of chronically elevated blood sugar or underlying prediabetes/diabetes.
- Have a Family History of Diabetes: If close family members (parents, siblings) have type 2 diabetes, your genetic predisposition is higher. Regular screening and early discussions with your doctor are advisable, even if you don’t have symptoms yet.
- Are Overweight or Obese: Being overweight or obese is a significant risk factor for insulin resistance and type 2 diabetes. If your Body Mass Index (BMI) is in the overweight or obese range, consulting a doctor about blood sugar screening and weight management strategies is a proactive step.
- Have Other Risk Factors: Conditions like high blood pressure, high cholesterol, or polycystic ovary syndrome (PCOS) are often linked to insulin resistance and increased diabetes risk. If you have any of these, regular blood sugar monitoring should be part of your health management.
- Are Pregnant or Planning Pregnancy: Gestational diabetes can develop during pregnancy and poses risks to both mother and baby. Early screening and management are vital. If you plan to become pregnant and have risk factors for diabetes, discussing this with your doctor beforehand is important.
- Are Concerned About Your Glucose Levels: Even if you don’t have obvious symptoms, if you’ve been monitoring your blood sugar at home and consistently see elevated readings (e.g., fasting glucose over 100 mg/dL or post-meal levels consistently over 140 mg/dL, consult your doctor for formal testing and evaluation.
- Experience Rapid or Unexplained Weight Loss/Gain: Significant and unexplained changes in weight can sometimes be a sign of metabolic imbalances, including diabetes.
- Are Unable to Manage Levels Despite Lifestyle Changes: If you’ve diligently implemented dietary and lifestyle modifications for a reasonable period (e.g., several months) and are still struggling to stabilize your blood sugar or your symptoms persist, it’s time for professional guidance to explore other options or deeper underlying causes.
- Recognize the Signs: Be aware of common symptoms like fatigue after meals, increased thirst, frequent urination, headaches, and brain fog, as well as less obvious indicators like skin changes or recurring infections, which can signal blood sugar spikes.
- Dietary Choices are Key: Prioritize whole, unprocessed foods rich in fiber, lean proteins, and healthy fats. Limit refined carbohydrates, added sugars, and oversized portions to prevent rapid glucose surges.
- Embrace a Healthy Lifestyle: Regular physical activity enhances insulin sensitivity. Effective stress management and consistent, adequate sleep are also crucial for maintaining stable blood sugar levels.
- Monitor and Understand: If you have risk factors or experience symptoms, consider monitoring your blood sugar to understand your body’s unique responses to food and lifestyle choices.
- Seek Professional Guidance: Don’t hesitate to consult a doctor, registered dietitian, or certified diabetes educator if you have persistent symptoms, risk factors, or concerns about your blood sugar levels for personalized advice and diagnosis.
#### Less Obvious Indicators
Beyond the immediate and more commonly recognized symptoms, there are several subtle indicators that might suggest ongoing or frequent blood sugar imbalances. These often point to a more chronic issue or the body’s attempts to cope with repeated glucose surges.
The Risks of Unmanaged Blood Sugar Spikes
While the immediate symptoms of a blood sugar spike can be uncomfortable and disruptive, the true concern lies in the long-term consequences of frequent and unmanaged glucose surges. These repeated fluctuations place significant stress on various bodily systems, incrementally increasing the risk of serious chronic health conditions. Understanding these risks underscores the importance of proactive management.
One of the most significant dangers is the progression of insulin resistance. When cells are repeatedly exposed to high levels of insulin in response to spikes, they can become less responsive over time. This means the pancreas has to produce even more insulin to achieve the same effect, creating a vicious cycle. Eventually, the pancreas may not be able to keep up, leading to persistently high blood sugar levels.
This unchecked progression dramatically increases the risk of developing prediabetes and type 2 diabetes. Prediabetes is a condition where blood sugar levels are higher than normal but not yet high enough to be diagnosed as type 2 diabetes. It’s a critical warning sign, as many individuals with prediabetes eventually develop type 2 diabetes if lifestyle changes are not implemented. Type 2 diabetes, once established, is a chronic condition that requires lifelong management and can lead to severe complications.
Beyond diabetes, unmanaged blood sugar spikes have a profound impact on cardiovascular health. High glucose levels can damage blood vessels and nerves that control the heart and blood vessels. Over time, this damage contributes to the hardening and narrowing of arteries (atherosclerosis), increasing the risk of high blood pressure, heart attack, and stroke. The inflammatory processes triggered by glucose spikes also play a role in this cardiovascular deterioration.
Nerve damage, or neuropathy, is another serious complication. High blood sugar can harm the tiny blood vessels that supply nerves, particularly in the extremities. This can lead to tingling, numbness, burning, or pain in the hands and feet. If left unaddressed, it can result in loss of sensation, increasing the risk of injuries and infections that go unnoticed.
The kidneys are also vulnerable. Frequent spikes can strain the tiny filtering units within the kidneys, leading to kidney damage (nephropathy). Over years, this can progress to chronic kidney disease, potentially requiring dialysis or a kidney transplant.
The eyes are not immune either. High blood sugar can damage the blood vessels in the retina, leading to diabetic retinopathy, a condition that can cause vision impairment and even blindness if not managed. Cataracts and glaucoma are also more prevalent in individuals with diabetes.
Even cognitive decline has been linked to long-term blood sugar dysregulation. Research suggests that chronic high blood sugar and insulin resistance can negatively affect brain function, increasing the risk of dementia and other neurodegenerative conditions. The brain relies on a stable energy supply, and the rollercoaster of spikes and crashes can be detrimental.
In essence, unmanaged blood sugar spikes are not merely a matter of temporary discomfort. They represent a significant physiological stressor that, over time, can erode health across multiple organ systems. Recognizing this broad spectrum of risks provides a powerful motivation for adopting strategies that promote stable glucose levels.
Causes and Triggers of Blood Sugar Spikes
Understanding why blood sugar spikes occur is fundamental to preventing them. Many factors, primarily related to diet and lifestyle, can contribute to these unwelcome fluctuations. By identifying common triggers, individuals can make informed choices to maintain steadier glucose levels.
#### Dietary Factors
What we eat, how much we eat, and when we eat are the primary drivers of blood sugar responses. Certain foods and eating habits are particularly prone to causing rapid glucose surges.
#### Lifestyle Factors
Beyond diet, several aspects of our daily lives can significantly influence how our bodies manage blood sugar. These lifestyle choices can either support stable glucose or contribute to unwanted spikes.
Practical Strategies to Prevent Blood Sugar Spikes
Preventing blood sugar spikes is a cornerstone of maintaining metabolic health and reducing the risk of chronic diseases. Fortunately, many effective strategies are within our daily control, primarily involving mindful dietary choices and consistent healthy lifestyle habits. Implementing these strategies can lead to more stable glucose levels, sustained energy, and improved overall well-being.
#### Dietary Approaches
The foods we choose and how we combine them are powerful tools in regulating blood sugar. Small, consistent changes can yield significant benefits.
Specific Food Combinations: The order in which you eat foods within a meal can also matter. Some evidence suggests that eating protein and vegetables before* carbohydrates can lead to a lower post-meal glucose response. This allows the protein and fiber to create a buffer in the stomach, slowing the entry of glucose into the bloodstream.
#### Lifestyle and Daily Habits
Diet is crucial, but comprehensive blood sugar management also relies on integrating healthy habits into your daily routine.
Monitoring Blood Sugar: For individuals at risk or those already managing prediabetes/diabetes, regular blood sugar monitoring (with a glucometer or continuous glucose monitor – CGM) can provide invaluable insights. This helps you understand how specific foods, activities, and stress levels impact your* glucose levels, allowing for personalized adjustments and a deeper understanding of your body’s responses.
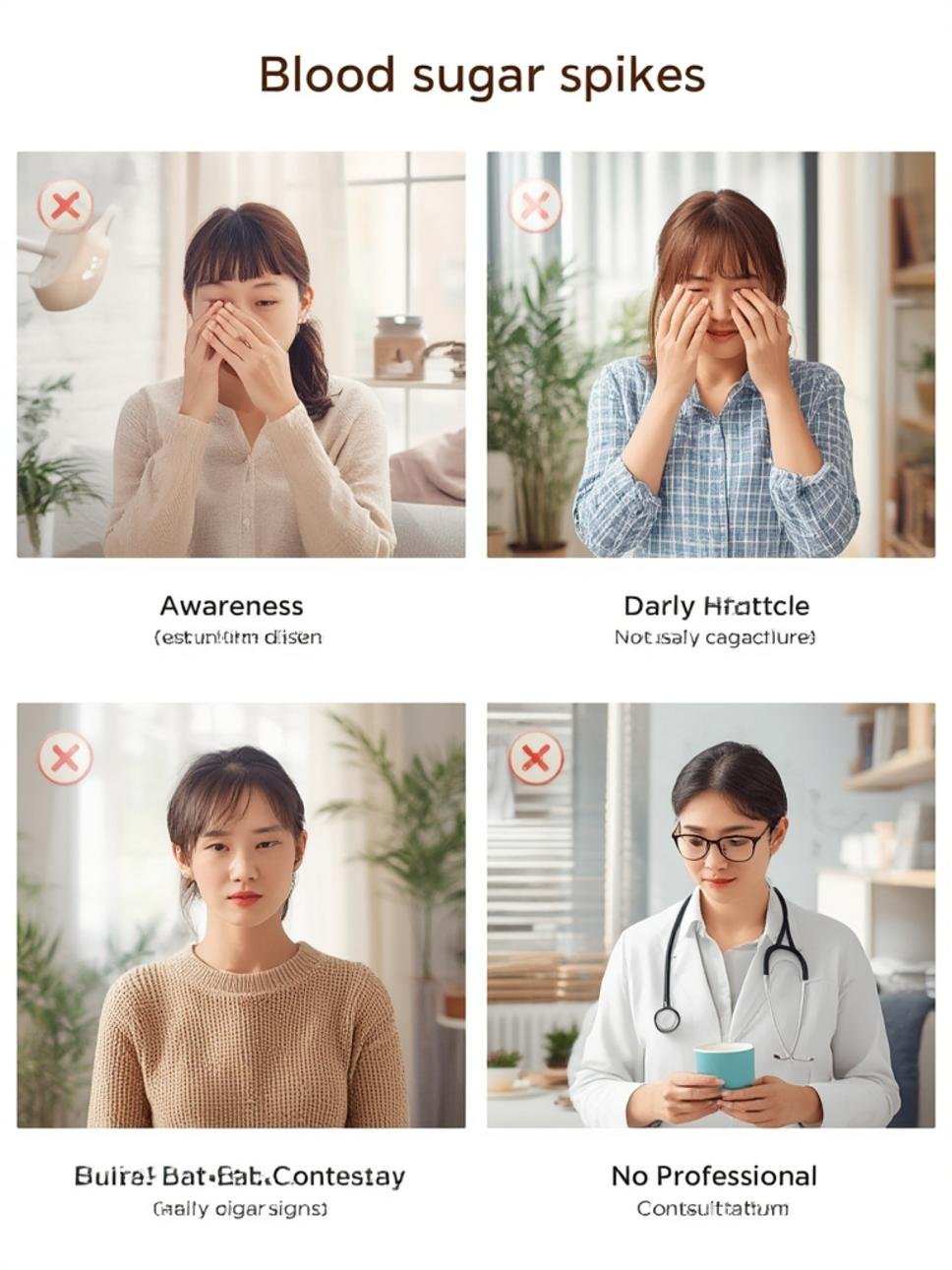
The Role of Professional Guidance
While many strategies for preventing blood sugar spikes are centered around lifestyle and diet, the importance of professional medical guidance cannot be overstated. Self-management is powerful, but a healthcare team can provide personalized advice, diagnostic clarity, and support, particularly for individuals experiencing persistent symptoms or those at higher risk.
Consulting with a doctor is the first crucial step if you suspect you are experiencing frequent blood sugar spikes or if you have concerns about your metabolic health. A medical professional can assess your overall health, review your medical history, and discuss your symptoms in detail. They can help differentiate between typical post-meal glucose fluctuations and patterns that indicate prediabetes or diabetes.
Regular check-ups are essential for monitoring various health markers, including blood sugar. During these visits, your doctor may recommend specific diagnostic tests to get a clearer picture of your glucose metabolism.
Based on these tests, your doctor can accurately diagnose conditions like prediabetes or diabetes and develop an appropriate management plan. This plan might involve specific dietary recommendations, exercise prescriptions, and, if necessary, medication.
Beyond your primary care physician, other healthcare professionals can offer invaluable support:
Working collaboratively with a healthcare team ensures that your blood sugar management strategy is comprehensive, evidence-based, and tailored to your individual needs. They can help you interpret your blood sugar readings, adjust your lifestyle interventions, and provide ongoing support and education to empower you in your health journey.
When to Seek Professional Advice
While proactive lifestyle changes can significantly improve blood sugar control, there are specific situations where seeking professional medical advice becomes particularly important. Delaying consultation can sometimes lead to the progression of conditions that are more challenging to manage later.
You should consider contacting a healthcare professional if you:
Remember, early detection and intervention for blood sugar dysregulation can prevent or significantly delay the onset of serious complications. A healthcare provider can offer clarity, accurate diagnosis, and a personalized plan to help you achieve and maintain optimal metabolic health.
FAQ Section
Q1: What is considered a “high” blood sugar reading after a meal?
A1: Generally, for individuals without diabetes, blood sugar levels typically peak under 140 mg/dL (7.8 mmol/L) one to two hours after a meal. Readings consistently above this, particularly above 180 mg/dL (10.0 mmol/L), would be considered a significant spike and warrant professional evaluation, especially if they occur frequently.
Q2: Can blood sugar spikes happen even if I don’t have diabetes?
A2: Yes, absolutely. Even individuals without a diabetes diagnosis can experience blood sugar spikes, especially after consuming meals high in refined carbohydrates and sugars. These spikes, particularly if frequent, can contribute to insulin resistance over time and increase the risk of developing prediabetes and type 2 diabetes.
Q3: How quickly do blood sugar spikes typically occur after eating?
A3: Blood sugar spikes usually occur within 30 minutes to two hours after eating, depending on the type and quantity of food consumed. Meals rich in simple carbohydrates and sugars tend to cause a faster and higher peak compared to meals balanced with fiber, protein, and healthy fats.
Q4: Is it normal to feel tired after eating, or is that always a sign of a blood sugar spike?
A4: While some post-meal drowsiness can be normal, especially after a large meal, profound fatigue, an energy crash, or “food coma” is often a strong indicator of a significant blood sugar spike followed by a rapid drop. Regular, intense post-meal tiredness, particularly after certain types of meals, suggests an imbalanced glucose response that warrants attention.
Q5: Can stress alone cause blood sugar to spike?
A5: Yes, stress can definitely cause blood sugar levels to rise, even without eating. When stressed, the body releases hormones like cortisol and adrenaline, which signal the liver to release stored glucose into the bloodstream, preparing the body for a “fight or flight” response. Chronic stress can lead to chronically elevated blood sugar.
Key Takeaways
Conclusion
Understanding and proactively managing blood sugar spikes is a fundamental aspect of safeguarding your long-term health. While the immediate effects might feel like mere inconveniences, chronic glucose imbalances can pave the way for serious health complications. By adopting mindful dietary practices, prioritizing an active lifestyle, managing stress, and ensuring sufficient sleep, you empower your body to maintain the delicate balance it needs. Remember, knowledge is power, and taking control of your blood sugar health is one of the most impactful investments you can make in your future well-being. Start today by making small, consistent choices that support stable glucose levels, and consider seeking professional advice to guide you on this vital journey.






