Gut Health: The Ultimate Guide to Probiotics, Prebiotics, and Your Mood
This guide explains how the microbiome links to the brain and why that connection matters for daily life.
We cover what fermented food and supplements do, how signals from the gut can affect the central nervous system, and why results vary across people.
Scientific evidence for probiotics and mood is mixed. Products sold in the U.S. are regulated as supplements, so strains and potency differ. Most options are safe for healthy adults, but effects are personal. A one-month trial is a reasonable way to test benefits without replacing prescribed care.
We also frame the topic within today’s mental health landscape and link to key resources so readers can learn more about stress, anxiety, and system-level support.
Key Takeaways
- The guide shows how the microbiome and brain communicate and why that link matters.
- Fermented food, supplements, and fiber play distinct roles in overall health.
- Evidence for direct mood change is promising but still limited; products vary.
- Use a one-month trial to assess personal benefit while keeping existing care.
- Pair dietary steps with stress management and sleep for more reliable results.
Foundations: How your microbiome, probiotics, and the gut-brain axis shape mood
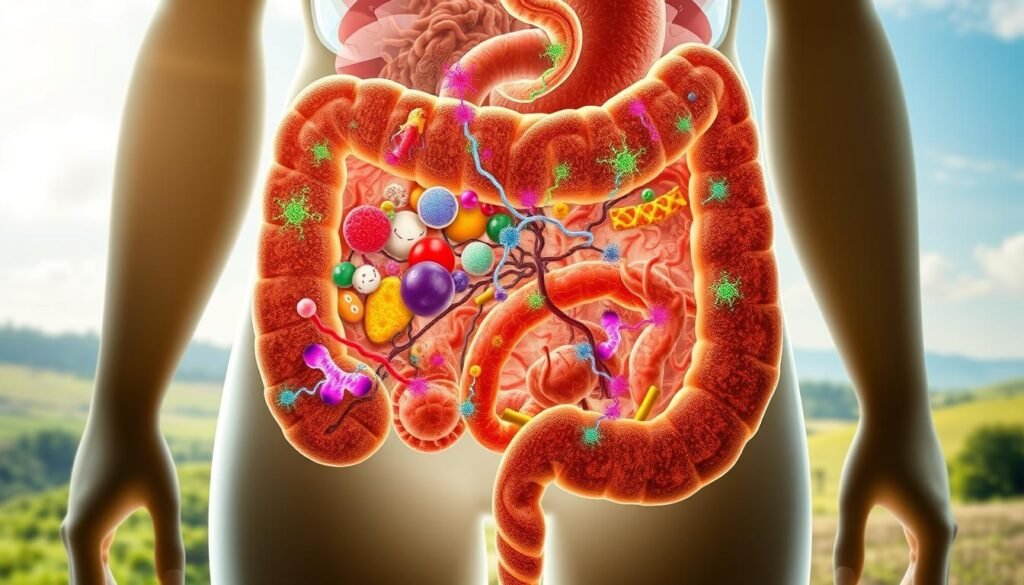
Foundational biology shows multiple routes by which microbes in the digestive tract can influence brain function.
What they are: Probiotics are live microorganisms you can consume; prebiotics are fermentable fibers that feed those microbes. Together they shape the digestive tract ecosystem and influence how the body processes signals.
How the enteric network communicates
The brain and nervous system receive messages from the digestive tract via three main routes: the vagus nerve, immune system signaling, and hormonal messengers. This bidirectional link is often called the enteric nervous or the “second brain.”
Why strain and source matter
Different genera—Lactobacillus and Bifidobacterium—contain distinct bacteria with unique functions. That is why probiotics work differently by strain and why labels with strain names and “live and active cultures” matter.
Public health context
Stress and anxiety remain widespread; authoritative pages from WHO (https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response), NIMH (https://www.nimh.nih.gov/health/topics/anxiety-disorders/index.shtml), and the APA (https://www.apa.org/topics/stress/managing) show why foundational knowledge of this connection supports broader care strategies.
- Sources: yogurt, kefir, kimchi, sauerkraut, miso, kombucha, and some cheeses list live cultures.
- Survival: microbes must survive the stomach to reach the intestines; formulation and storage affect outcomes.
- Expectation: quality, strain choice, and consistent intake shape likely benefits; individual responses vary.
Evidence review: gut health, probiotics and mood
Emerging research shows that study design often decides whether small psychological effects are detected.

What current research shows about changes in feelings
A randomized, double‑blind trial of 88 healthy adults gave a multispecies probiotic for four weeks. Standard questionnaires found little change, yet daily ratings showed reduced negative feelings starting around two weeks.
Why daily tracking matters
Frequent, real‑time ratings capture nuance that weekly surveys miss. A recent JMIR 2024 commentary explains how measurement frequency alters conclusions about small effects.
Who may benefit and plausible pathways
People with higher risk aversion or mild symptoms saw larger gains, suggesting early support for specific subgroups.
Possible mechanisms include immune modulation, vagus nerve signaling, and hormonal routes that affect emotional processing in the brain, as summarized in a 2024 PMC review.
| Aspect | Finding | Timeline | Notes |
|---|---|---|---|
| Daily ratings | Reduced negative affect | ~2 weeks | Sensitive to small changes |
| Standard questionnaires | Minimal change | 4 weeks endpoint | May miss transient effects |
| Who benefits | Risk‑averse individuals | Early response | Subgroup effect; needs replication |
| Safety & regulation | Generally safe for healthy adults | Ongoing | Strain, dose, and viability vary; supplements not regulated as drugs in the U.S. |
Bottom line: A probiotic may offer modest, measurable support when outcomes are tracked often. These products work best as an adjunct to lifestyle and clinical care, not as standalone treatments.
Practical strategies to improve your gut and support mood—foods, supplements, and habits
Simple plate swaps and brief stress tools often yield clearer signals than a single supplement trial. Start with a fiber‑forward plate: vegetables, legumes, whole grains, nuts, and seeds. Add fermented foods such as yogurt, kefir, sauerkraut, kimchi, miso, or cottage cheese that list live and active cultures.

Selecting a supplement like a clinician
Look for named strains (for example, L. rhamnosus GG or B. longum), clear CFU counts, storage instructions, and an expiration date. Remember that products sold as supplements vary by strain and viability; match the label to your goal.
Timing, expectations, and safety
Try one product daily for about four weeks. Track comfort after meals, stool form, energy, and emotional steadiness. If nothing improves, consider switching strains and consult your clinician before changing any treatment—especially with irritable bowel syndrome or mood conditions.
Stress, screen time, and routine
Use APA stress techniques and brief mindfulness exercises (see Psychology Today). Reduce screen load with stepwise digital detox tips from Greater Good and Lifeline. Favor quality protein per Harvard guidance and Blue Zone patterns to build resilience.
- Eat diverse plants and rotate fermented foods.
- Choose supplements with named strains and proper CFU.
- Pair trials with stress tools and clinician oversight.
Conclusion
Short trials with clear tracking give the best insight. Try a named-strain supplement for about four weeks while noting daily changes in appetite, bowel comfort, energy, and mood. This helps spot modest effects that surveys can miss.
Use a whole-person plan: a nutrient-dense plate, regular movement, sleep, and brief stress tools. Quality matters—look for named strains, proper CFU, storage, and an expiration date so live bacteria are likely to survive the stomach and reach the digestive tract.
If you live with anxiety, depression, or irritable bowel syndrome, work with your clinician. For trusted guidance, see WHO, NIMH, and APA resources listed above to shape safe, evidence-informed next steps.






